Image Guided Minimally Invasive Spine Surgery
When you first begin to learn surgery, the thing that's drummed into your head is "visualization"..., being able to SEE what you are operating on. Visualization is one of the main reasons that spine surgery in the past could require large incisions. In some cases, incisions might be as long as 12 inches or more. Needless to say, this meant cutting through a great deal of healthy muscle and tissue to be able to see the surgery site. Large incisions meant increased blood loss, and extended recovery times.
One of the most important innovations in spine surgery has been the introduction of "Image Guided Surgery". New technology and low dose radiation techniques now allow us to "visualize" without actually making a large incision. (and low dose is at least as important to me as it is to you. I use this technology regularly)
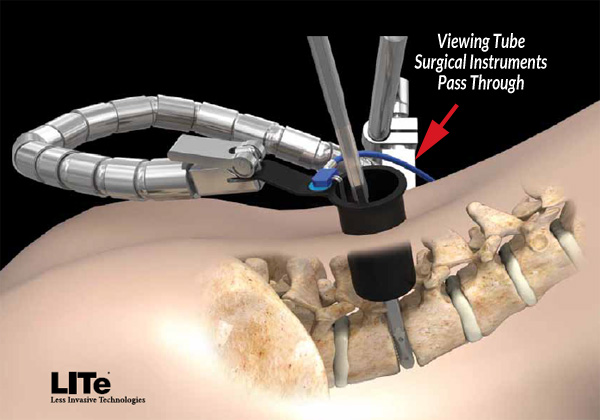
Here's how it works. The O-arm surround the patient and the operating table. By taking a "continuous" x-ray, the surgeon can see exactly what's happening, but without the necessity of a large incision. Surgical instruments can be guided strictly through the use of images. The result is Minimally Invasive Spine Surgery, where we can work with the minimum required incision..., really, just large enough to admit the surgical instruments.
The following photos will illustrate how the system works. If you have questions about its effectiveness or suitability for your condition, please contact the practice for an evaluation. We're committed to the idea that educated patients have the best outcomes.
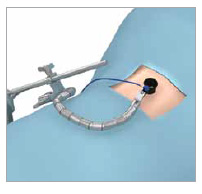
The incisions for surgery with LITe® are small.
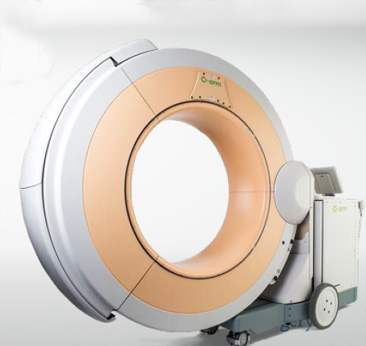
The O Arm which "takes" the pictures.
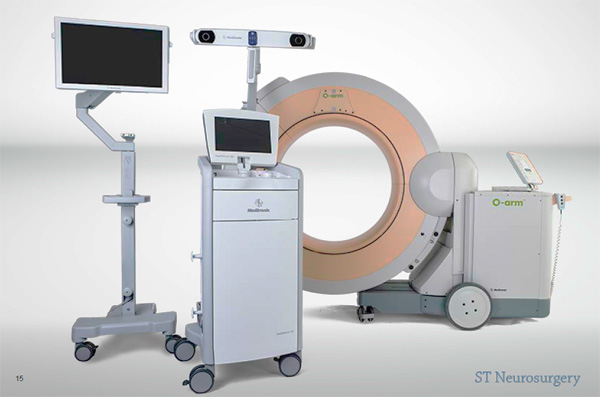
The computers and viewing station.

The Complete System
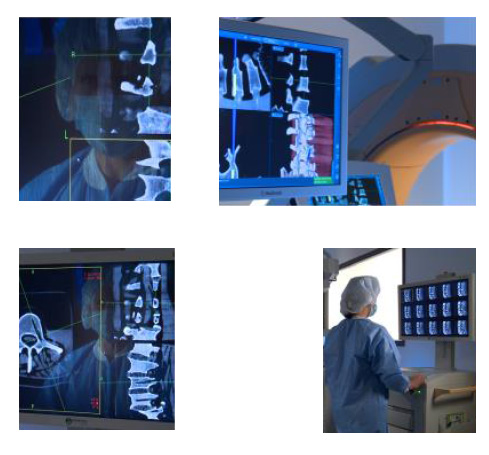
What the Surgeon Sees
The Stealth System is a powerful technology for advancing the availability of Minimally Invasive Spine Surgery.
We place the tube through which the surgery is conducted. In some cases, the tube can be as small as half an inch in diameter.
Below is an approximation of what the surgeon sees during the surgery. As you can see, the point of MIS is to limit the size of the incision to what is actually required to complete the surgery safely and effectively.

If you were in the OR, this is what the surgery looks like.
ACUTE - CHRONIC - EPISODIC
Typically back pain originates in the neck (cervical), mid back (thoracic), low back (lumbar), or a combination such as 'thoracolumbar pain'. Depending on the source of the pain, certain types of pain may be indicative of disease or a particular disorder.
Pain may be described as sudden, sharp, persistent, or dull. Symptoms may be localized to a specific area of the back (e.g. neck) or may radiate into the shoulders, arms, low back, buttocks, legs, and even the feet. Sometimes pain is accompanied by neurologic symptoms such as numbness, tingling, or weakness.
Back pain is either acute or chronic. Acute pain may begin suddenly with intense pain usually lasting a short period of time. Chronic pain is persistent long-term pain, sometimes lasting throughout life. Even chronic pain may present episodes of acute pain.
Certain neurologic symptoms may indicate the need for immediate medical attention. These 'red flags' include bowel or bladder dysfunction, extremity weakness or numbness, severe symptoms that do not subside after a few days, or pain that prohibits everyday activities.
A MYRIAD OF CAUSES
A cause of back pain is muscle strain and spasm. Strain may result from the 'weekend warrior syndrome', heavy physical work, awkward bending or twisting, even poor posture.
Whiplash
is neck pain, which commonly occurs following an auto accident. This is typically caused by hyperextension and/or hyperflexion because the head is forced to move backward and/or forward rapidly beyond the neck's normal range of motion. The unnatural and forceful movement affects the muscles and ligaments in the neck. Muscles may react by tightening and contracting, creating muscle fatigue, resulting in pain and stiffness.
Osteoarthritis (Spondylosis)
Spinal osteoarthritis, or spondylosis, is a degenerative disorder that may cause loss of normal spinal structure and function. Although aging is the primary cause, the location and rate of degeneration is individual. The degenerative process may impact the cervical, thoracic, and/or lumbar regions of the spine affecting the discs and spinal joints.
Osteoporosis
Osteoporosis commonly affects the thoracic and thoracolumbar regions of the spine and may cause debilitating pain. This disorder is caused by a loss of bone mineral density resulting in fragile bones, which may fracture. Osteoporosis may cause vertebral compression fractures, loss of height, stooped posture, even a humped back. The patient can control some of the risks for osteoporosis. These include poor diet, smoking, excessive intake of alcohol, and inactivity.
Herniated Disc
A disc herniation is a disc rupture. This may occur if the nucleus pulposus (gel-like center) erupts through the annulus fibrosus (protective disc wall) or if the annulus fibrosus fragments. The progression to an actual herniation varies from slow to sudden onset of symptoms.
There are four stages:
(1) disc protrusion,
(2) prolapsed disc,
(3) disc extrusion, and
(4) sequestered disc.
Stages 1 and 2 are referred to as incomplete, where 3 and 4 are complete herniations.
Sciatica
The term 'sciatica' is commonly used to describe pain that travels along the sciatic nerve, the largest nerve in the body. The pain may be sharp, dull, burning, or accompanied by intermittent shocks of shooting pain beginning in the buttock traveling downward into the back of the thigh and leg. The most common cause of sciatica is a herniated disc in the lumbar spine.
Compression Fracture
A compression fracture is a common fracture of the spine that may range from mild to severe. Each vertebral body is separated from the other with a disc. When an external force is applied to the spine, such as from a fall or carrying a sudden heavy weight, the forces may exceed the ability of the bone within the vertebral body to support the load. This may cause the vertebral body to crush. This is known as a compression fracture. If the entire vertebral body breaks, this is considered a burst fracture.
Spinal Stenosis
Spinal stenosis results when the small neural passageways termed 'foramen' narrow. The narrowing of the foramen may compress and entrap nerve roots. Nerves react to pressure by swelling, which further reduces foraminal space. Stenosis can cause excruciating pain, numbness, tingling, or burning in the involved extremity (e.g. leg, arm). Stenosis can also occur with compression from a disc, osteophytes (e.g. bone spurs), and ligaments.
Scoliosis
Scoliosis causes the spine to curve laterally to the left or right and affects children and adults. Scoliosis is a complex three-dimensional disease. To understand this concept, consider that in some cases, as the spine abnormally curves, the involved vertebrae are forced to rotate. At the thoracic level, vertebral turning impacts the rib cage and may result in rib prominence on the opposite side of the curve. Deformity is the primary complaint. Back pain from scoliosis is uncommon.
Spinal Infections (Osteomyelitis)
Osteomyelitis is a bone infection usually caused by bacteria. In the spine it is commonly found in the vertebrae, although the infection can spread into the epidural and/or intervertebral disc spaces. Typically, symptoms include persistent and severe back pain exacerbated by movement, swelling, fever, sweating, weight loss, and malaise.
DETERMINING THE CAUSE
Back pain is not always indicative of a spinal problem. Rarely is back pain an emergency or serious medical condition. A proper diagnosis is paramount to determine the best course of treatment. A thorough physical and neurologic assessment may reveal the cause of the pain.
The examination begins with the patient's current condition and medical history. The oral segment of the examination often includes many questions such as "when did the pain start?" - "what activities preceded the pain?" - "previous treatment" - "does the pain radiate or travel into another part of the body?" - "what makes the pain less or greater?" - and so on.
This examination includes observation of the patient's posture, range of motion, and physical condition. Any movement generating pain is noted. The physician will palpate or feel the curvature of the spine, vertebral alignment, detect muscle and tender points. Abdominal palpation may be performed to determine if the cause of low back pain is possibly internal organ related (e.g. pancreas).
The neurological examination tests the patient's reflexes, muscle strength, detects sensory and/or motor changes, and determines pain distribution. If nerve damage is suspected, the physician may order special tests to measure the rate at which nerves conduct impulses. These tests are termed Nerve Conduction Velocity (NCV) and Electromyography (EMG). Typically these studies are not performed immediately because it may take several weeks for nerve impairment to become apparent.
If infection, malignancy, fracture, or other risk factors are suspected, routine lab tests may be ordered. These tests may include complete blood count (CBC), erythrocyte sedimentation (ESR), and urinalysis.
Plain radiographs (x-rays), CT Scan, and/or MRI studies are performed when fracture or disc disease is suspected, or to evaluate neurologic dysfunction. An MRI represents the gold standard in imaging today. An MRI renders high-resolution images of spinal tissues such as the spinal cord and intervertebral discs. X-rays are still the imaging method of choice to study the bony elements in the spine.
NONSURGICAL - CONSERVATIVE TREATMENT
Seldom does back pain require surgical intervention. A conservative treatment plan may include bed rest for a day or two combined with medication to reduce inflammation and pain. Medications recommended by the physician are based on the patient's medical condition, age, other drugs the patient currently takes, and safety.
The first choice for pain relief is often nonsteroidal anti-inflammatory drugs (NSAIDs). These drugs should be taken with food to reduce the risk of stomach upset and stomach bleeding. Muscle relaxants may provide relief from muscle spasm but are actually benign sedatives, which often cause drowsiness. Narcotic pain relievers may be prescribed for use during the acute phase.
A cervical collar may be recommended to help a patient with neck pain. Cervical collars limit movement and support the head taking the load off the neck. Lying down has a similar affect. Limiting neck movement and reducing pressure (weight) gives muscles needed rest while healing. Cervical traction may be prescribed for home use. This form of traction gently pulls the head, stretching neck muscles, while increasing the size of the neural passageways (foramen).
Physical Therapy (PT) may be incorporated into the patient's treatment plan once activity can be tolerated. PT may include ice therapy to slow nerve conduction thereby decreasing inflammation and pain. Heat treatments may be used to accelerate soft tissue repair. Heat increases blood flow and speeds up the metabolic rate to assist healing. Heat also helps decrease muscle spasm, pain, and promotes a relaxed feeling. Ultrasound is a treatment used to deliver heat deep into soft tissues. Sometimes a heat treatment is given prior to a session of therapeutic exercise.
Therapeutic exercise can help build strength, increase range of motion, coordination, stability, balance, and promotes relaxation. Therapists educate their patients about their condition and teach posture correction and relaxation techniques. Patients who participate in a structured physical therapy program often progress to wellness more rapidly than those who do not. This includes back maintenance through a home exercise program developed for the patient by the physical therapist.
SURGERY - SELDOM REQUIRED
Seldom is surgery required to treat back pain. Indications for surgery include, but are not limited to spinal cord dysfunction, bowel and/or bladder dysfunction, excruciating pain (more often leg pain is greater than back pain) unrelieved by non-operative measures, and prolonged pain and/or weakness.
RECOVERY and PREVENTION
First and foremost, follow the treatment plan outlined by the physician and physical therapist. Patients, who undergo a surgical procedure, may find the road to recovery a bit longer. However, that is not reason to become discouraged. It is normal to feel tired and emotionally down following surgery. During stress such as surgery, the body cranks out extra hormones - after surgery the level drops, which may result in a 'down' period. To enhance recovery from surgery, an episode of back pain, or to help minimize future exacerbation try to maintain good posture, be consistent in a home exercise program, and eat sensibly to maintain proper body weight.
